 ’Round the Circle-Game We Go
’Round the Circle-Game We GoDepartment of Public Health’s Dialysis Crisis
Article Printer-friendly
PDF file
Westside Observer (In Press)
October 2013 at www.WestsideObserver.com
Dedicated to Jimmy Manges
 ’Round the Circle-Game We Go
’Round the Circle-Game We Go
Department
of Public Health’s Dialysis Crisis
by Patrick Monette-Shaw
For more than 46 years, dialysis services have been admirably provided on the campus of San Francisco General Hospital. But in a move to privatize every public service it can, the City is making a dire mistake outsourcing dialysis to the private sector, and placing it at Laguna Honda Hospital.
Although the Department of Public Health likes to boast that it is “integrating” patient care between SFGH, LHH, and its many community-based clinics throughout the City, DPH is about to fracture the delivery of services for dialysis patients who have been treated on SFGH’s campus for nearly half a century, after the State of California first awarded a grant to UCSF’s Medical Center to establish the UC Renal Center at SFGH in 1967.
Following the dialysis center’s opening shortly after receiving the State’s grant, it has faced a growing circle of licensing and financial-loss problems, and then faced chronic indecision regarding its fate from UCSF, SFGH, the Department of Public Health, and mostly from San Francisco’s governing Health Commission.
Coming
full circle, the decision to outsource dialysis services to an
outside contractor and place a 30-chair outpatient dialysis center
in Laguna Honda Hospital’s seismically unsafe old main buildings
is extremely troubling, when not potentially dangerous to patient
safety, as the Observer first reported in our September issue (“Squished
Together: Misery Visits Company”).
The Licensure Circle
After operating the UC Renal Center at SFGH for 33 years, the broader UCSF Medical Center notified SFGH in 2001 that it would no longer license the Renal Center at SFGH. A year later, UCSF’s Department of Medicine at SFGH luckily stepped in and became independently licensed to operate the UC Renal Center at SFGH. But a year following that, in 2003 UCSF’s Department of Medicine unsuccessfully tried to sell the facility, or partner with a private company, due to its financial losses. So in 2003, the facility and its license were transferred to SFGH, and the unit was renamed the SFGH Renal Center, where it has operated for the past decade.
And during that same past decade, since Katie Worth published several articles in the San Francisco Examiner in 2004 about the chronic shortage of dialysis services all over San Francisco in both the public and private sectors, debate — and constant indecision and delay — has raged about placing dialysis services at LHH, despite initial plans to rebuild both LHH and SFGH without any dialysis services in either of the replacement hospitals.
A
current Request
for Proposals to outsource SFGH’s dialysis services specifically
requires that the entity who is awarded a ten-year contract will
be responsible for obtaining licensure to operate outpatient dialysis
services at LHH. As far back as 2007, the State agency that issues
licenses for dialysis services prohibited long-term care nursing
facilities from operating a dialysis center on site. But in early
2007, the State Assembly quickly authored AB 214 to permit long-term
health care facilities to provide chronic dialysis clinic services
to residents of their facilities. Notably, AB 214 did not authorize
the skilled nursing and long-term facilities to operate outpatient
dialysis centers, just services for inpatient residents.
By 2009, the State Assembly introduced AB 1544, to expedite approval of new outpatient clinics without a prior onsite survey, but the bill initially would have prohibited acute care hospitals, psychiatric hospitals, and specialty hospitals from providing new outpatient services for chronic dialysis treatment. As AB l1544 wound through the State Senate, amendments to the bill on September 4, 2010 struck out the prohibition restricting outpatient dialysis services from the bill.
To our knowledge, LHH has never tried to obtain a license to provide any dialysis services, and indeed, its current license and menu of “clinics” does not include inpatient dialysis. Notwithstanding its lack of license for dialysis services, change orders were eventually approved during construction of LHH’s new facilities, adding a six-chair dialysis center that was built out on the promenade in LHH’s new Pavilion building, and dialysis chairs and equipment were purchased and delivered, although the small inpatient dialysis clinic has not opened in the three years since LHH moved into its new digs. Many of LHH’s current and former staff were never informed the six-chair dialysis unit was even there waiting to be opened, but never was. As a result, LHH’s dialysis patients still endure being transported to SFGH’s Renal Center for treatment.
Sources
report that despite the construction of a six-chair inpatient
dialysis center in LHH’s new Pavilion building, former Director
of Public Health Mitch Katz would not allow LHH to open it, for
fear of taking away business from SFGH. “Doctors don’t
like losing dialysis patients because the business is very lucrative,
and competition for Medicare patients is fierce,” a former
LHH physician speaking on condition of anonymity notes.
Similarly, LHH’s expansion of its acute physical medicine rehabilitation beds to 15 never panned out, as this reporter previously predicted might fail, because competition for acute rehab patients is also cut-throat among private hospitals. LHH’s share of the acute-care physical medicine rehab patient pie typically hovers at an average of no more than two at any given time, given the fierce competition for Medicare Part A acute rehab patients.
After receiving an additional $1.5 million or more annual budget increase to increase staff for a 15-bed acute rehab center planning to compete for Medicare Part A revenue that LHH’s Chief of Rehabilitation Services Lisa Pascual, MD asserted would occur — and which budget increase was approved by a beguiled Mayor and Board of Supervisors — LHH hasn’t been able to fill up more than half of its currently-licensed five acute rehab beds (not 15) at any one given time. LHH has failed so far to increase its grasp of the acute-care rehab reimbursement pie.
Lamely, a presentation to the SFGH Joint Conference Subcommittee on February 14, 2012 presented by SFGH’s CEO, Sue Currin and others, claimed on the “Funding Plan” slide that the six-chair inpatient dialysis unit was dropped from LHH’s rebuild plans in 2008 due to the projected high operational costs. But why would they have built out the six-chair unit and had the equipment delivered in 2010 if it had already been dropped in 2008? Knowledgeable sources believe it was never dropped from the plans, but that Dr. Katz refused to let it open and Currin was merely spouting spin control in 2012.
The Really-Bad-Location Circle
There are a number of reasons why moving SFGH’s dialysis center to Laguna Honda is a really bad location.
First, and foremost, it will fracture the care of dialysis patients, who attend multiple primary- and specialty-care appointments at SFGH each month, in addition to their weekly dialysis sessions. SFGH’s dialysis patients are among the most vulnerable in the City, suffering from ESRD, diabetes, congestive heart failure, cancer, HIV/AIDS, heroin addiction, and tuberculosis. Many patients require multiple SFGH-based clinic appointments, along with their three- to four-hour dialysis treatments three times a week.
The vast majority of dialysis patients treated at SFGH are African-American, Hispanic, or Asian/Pacific Islanders, most of them poor people already facing well-known disparities in access to medical care.
SFGH is the only dialysis unit in the city that accepts patients on gurney’s and from other community skilled nursing facilities who cannot ambulate due to quadriplegia, stroke, and vascular disease. It is also the only dialysis unit that accepts patients with aggressive behavioral issues who have failed at, or have been terminated by, other dialysis units in the City, and it is the only dialysis unit that accepts incarcerated patients needing dialysis who have lost medical insurance once in jail. It is the only unit in the City that dialyzes behavioral health patients (e.g., schizophrenia) and those requiring 24-hour care at SFGH’s secure facilities, since attempts to dialyze them at other units were unsuccessful, disruptive to other dialysis patients and staff, and costly, incurring both transportation costs and costs of safety “sitters” to accompany patients.
SFGH’s
Renal Center dialyzes patients who can’t be referred to private
centers, including those with paralysis, those on breathing tubes,
and those ineligible for insurance.
In December 2011, SFGH’s Renal Center received additional funding to staff a fourth evening dialysis shift specifically to address the problem of uninsured patients who are kept in the hospital at huge expense, because no other units in the City will accept them and the Renal Center did not have open chairs.
What will happen to all of these patients, since there is nothing in the RFP that stipulates that the vendor awarded the contract to operate a dialysis center at LHH will be required to accept these types of patients?
Moving the service to LHH will require these patients to obtain care at multiple locations, fragmenting their care between locations, and increasing the odds that they may end up admitted to SFGH’s emergency room. Many dialysis patients see multiple providers at SFGH during their dialysis visits, so they may end up making multiple trips to different campuses each week to receive fragmented care.
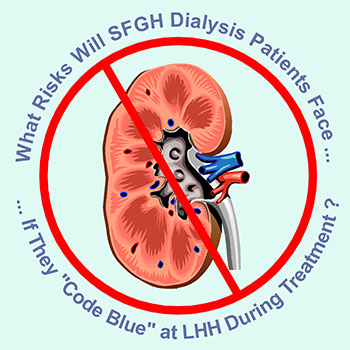
Second, the current Renal Center at SFGH formerly used ambulance transport when patients experience a medical emergency during dialysis treatment. Then, Renal Center staff learned they could use SFGH’s “Medical Emergency Response Team” (MERT), to use wheelchair transports from Ward 17 in Building 100 where the Renal Center is located, to transport patients by wheelchair quickly to SFGH’s E.R. along hallways in SFGH’s current main hospital in Building 5.
But there is no MERT at LHH, and the best LHH may offer be able to offer is use of its medical-staff Code Blue Team, who will have to travel a long distance on LHH’s campus from the new buildings were they see patients, over to the old main building where the outpatient dialysis center is proposed to be placed on the third floor. Alternatively, should patients Code Blue during dialysis treatment at LHH, following a delay in calls to 9–1–1, not only will there be an increase in fire alarms going off, the Fire Department station on Olympia Way behind LHH has no access road to LHH, and fire engines will be a three-minute ride away, barreling down Clarendon Avenue sirens ablaze, then along Laguna Honda Boulevard, before they can turn onto the grounds of LHH. If a Code Blue patient needs transport to the E.R. at SFGH, factor in at least a 10- to 15-minute trip to Potrero Avenue, causing further delays in care en route.
It is thought that SFGH’s MERT team is summoned to its Renal Center an average of three to four times a month for emergency transport, and Code Blue’s occur about six times annually.
Third,
moving dialysis services to LHH will exacerbate transportation
burdens. Studies have long documented that patients have poorer
outcomes the farther they have to travel to a dialysis center.
MediCal no longer reimburses for van transportation, although
MediCare does (and it is thought about 40 percent of SFGH’s
MediCare patients are quickly referred to other off-site dialysis
centers, and aren’t in SFGH’s on-site dialysis patient
mix). Anthem Blue Cross, which provides managed MediCal, does
not reimburse for transportation, nor does it reimburse for some
dialysis-related medications. It is not yet known whether the
San Francisco Health Plan or the separate Healthy San Francisco
programs cover transport costs.
Presentations made by DPH to the full Health Commission in February and April 2012 document that of 97 dialysis patients being treated at SFGH, 33 rely on public transportation, only 40 had an “entitlement van,” 4 rely on gurney transport in an ambulance, three walk, 12 have private cars, one is transported from jail by the Sheriff, and 4 were behavioral health patients presumably at SFGH’s Mental Health Rehab Facility at SFGH.
Worse, DPH’s presentation also noted that of 33 dialysis patients treated at SFGH who rely on public transportation, fully 26 (79 percent) reside in five zip codes in the Inner Mission, Bay View-Hunters Point, South of Market, Outer Mission, and Tenderloin neighborhoods, who will face an increase of 2.3 to 3.8 miles in public transportation to LHH, presumably with longer transit times, particularly from the Inner Mission and Bay View-Hunters Point.
As far as that goes, of the 97 dialysis patients seen at SFGH, fully 86 (89 percent) are from these same five neighborhoods, plus Bernal Heights and the Excelsior. Of SFGH’s additional 132 patients treated off site in the community, fully 98 (74 percent) are from these seven neighborhoods. Whether the 132 use public transit or other transportation, they will all face longer transportation times, in addition to their three- to four-hour dialysis treatments — assuming there are no delays in treatment that may affect missing scheduled van transport times for return home.
Patient
advocates fear SFGH’s dialysis patients may not be able to
endure two-hour bus rides, three times a week for dialysis.
Data in the presentation to the Health Commission is echoed by dialysis caregivers throughout the City. SFGH Renal Center staff have testified at Health Commission meetings that 90 percent of their patients live on the East Side near SFGH. They testified that the Laguna Honda site will pose access issues for Renal Center patients, all of whom receive primary and specialty care at SFGH. They don’t believe any SFGH outpatient services should be moved to LHH.
They note moving the Renal Center to LHH will mean increased van, car, ambulance, and pedestrian traffic in the LHH neighborhood. With just 99 dialysis patients treated three times each week (assuming that dialysis patients currently treated at community sites will remain where they are, despite DPH’s hope to move them to LHH, which likely won’t happen), there would be fewer than 198 round-trip transports three times each week, but there will still be a high number of vans running through the LHH neighborhood daily, which increase in traffic may not have even been considered when the Environmental Impact Report was prepared prior to construction of LHH’s replacement facility. This excludes SFGH’s 132 patients who are currently served off-site, and may or may not be forced to switch from community-based dialysis clinics, to LHH, which may exacerbate their transportation problems, and who may also be forced to change their nephrologists.
During testimony at the SFGH Joint Conference Subcommittee meeting of the Health Commission February 14, 2012, one member of the public testified that LHH was too far away, which may deter patients from getting the appropriate care; he read a letter into the meeting minutes from a medical transport company who stated that it can’t afford to transport patients to LHH due to lower reimbursement rates from MediCare.
The Chronic Indecision Circle
There has been little to no public discussion of the pros and cons of outsourcing SFGH’s dialysis services to LHH.
There has been no substantive discussion of the RFP to move dialysis to LHH at the full Health Commission. In response to a records request placed by this columnist on September 14, 2013, Health Commission Executive Secretary Mark Morewitz responded that there were no responsive documents to a records request for any “Resolution” adopted by the full Health Commission authorizing DPH to issue an RFP to outsource and privatize the Renal Center at SFGH and relocate those services to LHH.
Nor were there any responsive records for meeting minutes of the full Health Commission in which it formally approved DPH’s proposal to relocate the dialysis services to LHH. Morewitz also noted that there were no responsive documents to a request for any DPH budget initiative forms to eliminate dialysis services; he indicated no reductions have been made to the DPH outpatient dialysis budget. At least not yet.
Mr. Morewitz creatively tried to assert that DPH’s “outpatient dialysis services located at SFGH are currently ’outsourced’ to UCSF.” But it is thought that he’s stretching the truth, because the license for SFGH’s Renal Center resides with SFGH, not with UCSF. Although the Renal Center is staffed with UCSF employees, so are large areas throughout the SFGH medical center campus, and the employees are staffed under a so-called (and financially lucrative) “Affiliation Agreement” with UCSF, which is typically afforded cost-of-living and cost-of-doing business budget increases each year funded by DPH’s budget through the City’s General Fund. Unlike the Affiliation Agreement now in place to staff the SFGH-licensed Renal Center, the pending RFP will actually outsource the entire operation, including licensure, to an outside entity, even though the UCSF Department of Medicine’s Nephrology Division will retain control of “medical direction” for any outpatient dialysis center at LHH.
Morewitz
did, however, send along minutes of the Health Commission’s
SFGH Joint Conference Subcommittee meetings on held on February
14, 2012 and April 10, 2012. Scattered throughout both
SFGH JCC minutes, Health Commissioner Sanchez, PhD and Commissioner
Ed Chow, MD, repeatedly requested that DPH “explore all possible
options and postpone the release of the RFP [to move dialysis
to LHH] until Director [of Public Health Barbara] Garcia reports
back to the SFGH JCC regarding this issue.” There’s
no indication Ms. Garcia ever reported back.
For his part, Sanchez requested on February 14 that “DPH consider exploring other options so that outpatient dialysis services could remain on the SFGH campus, and another unit could be located at LHH” in order to continue serving safety-net patients if outpatient dialysis is moved to LHH. Despite postponing release of the RFP, it appears to have been issued, apparently without the requested report back from Garcia.
The minutes of the full Health Commission on April 17, 2012 report the SFGH JCC was “hopeful” a solution could be found regarding appropriate transportation to the new site for [dialysis] patients“ at LHH. This followed Dr. Chow’s helpful “suggestion” to ensure patient transportation be “part of the plan” in the SFGH JCC’s minutes of April 10, 2012. Unfortunately, the RFP to outsource dialysis to LHH mentions not one word about transportation issues, and the issue appears to have never crossed the lips of Barbara Garcia and the Health Commission before the RFP was issued, unless such conversations occurred behind closed doors, out of ear-shot and oversight of members of the public, and the very dialysis patients DPH purports to serve.
For her part, Health Commission President Sonia Melara said not one word about the issue on February 14, 2012, unless Morewitz elided her oral remarks from the “Commissioner Comments Follow-Up” section of the JCC’s published minutes. Melara, employed by St. Francis Hospital, may fully understand not wanting to divert lucrative MediCare dialysis patients from private sector providers vying for the fierce competition for dialysis revenue. She also holds an appointment as the Health Commission’s representative on the Board of Directors of the San Francisco Public Health Foundation, which also may be eager to preserve lucrative business for private-sector hospitals.
Fast forward to the SFGH JCC’s meeting on April 10, 2012. Once again, SFGH CEO Sue Currin presented a PowerPoint presentation to the JCC about outsourcing SFGH’s Renal Center. The April 10 minutes also report in the Commissioner Comments/Follow-Up section show that Commissioner Chow asked for “clarification on the reason for the timing of the review” of the [outsourcing] issue.“ Chow asked if DPH and SFGH had spoken “with UCSF about the Mt. Zion option or about the RFP [to outsource to LHH].” Cathryn Thurow, a UCSF Assistant Dean reported there had been no direct conversation with Mt. Zion, but indicated another UCSF Associate Dean — Dr. Sue Carlise — had spoken to UCSF administration and had “heard favorable feedback about it [UCSF] applying for the [LHH dialysis] RFP.”
Commissioner
Sanchez again stated he was “very interested” [apparently
as a UCSF employee himself], in “SFGH/DPH pursuing dialogue
with the UCSF leadership,” about any potential for UCSF “to
combine renovations of the SFGH and Mt. Zion outpatient renal
centers into one project to alleviate the need to move the unit
out of SFGH.” A week later, on April 17, in a summary report
of JCC Committee reports to the full Health Commission, Sanchez
commented that the goal is to find a safe facility to provide
dialysis services, and that he “would like the SFGH campus
to be part of a solution in regards to final plans for DPH’s
outpatient renal services.”
Once again, minutes of the April 10 SFGH-JCC meeting and the April 17 full Health Commission meeting report not one peep out of Ms. Melara or Ms. Garcia. Sanchez must surely know that LHH is really not a “safe” facility.
Given the Health Commission’s and DPH’s indecision about where to place outpatient dialysis services to serve SFGH patients, the most obvious solution the City studiously ignored is right under their noses, suggested by UCSF employees staffing the Renal Center at SFGH: Delaying the RFP and moving the dialysis center into SFGH’s current Acute Hospital in Building 5 in which approximately 140,000 square feet of space will become vacant, and available (turf desperately being fought over), when SFGH’s new hospital under construction and nearing completion vacates Building 5, which is far more seismically safe than either the Renal Center’s current location in Building 100, or LHH’s almost-as-ancient seismically-unsafe buildings, as the Westside Observer noted in our September issue, and certainly much larger than the 8,500 square-foot space being proposed for dialysis at LHH. SFGH is where the Renal Center should be located, in order to provide the most seismically-safe, life-safety location, since LHH isn’t.
Renal
Center staff suggested that since SFGH plans to move its Rheumatology,
Dermatology, and other “clinics,” into the vacated space
in Building 5, the logical choice would be to find room in Building
5 to move the Renal Center into, too, given the many co-morbidities
facing dialysis patients who would benefit by not fragmenting
locations of care.
Commissioner Chow, having asked Garcia and SFGH to consider “all options,” never commented on an option to move the Renal Center to Building 5. Indeed, the Health Commission appears never to have discussed in public meetings, that Building 5 might well be the best location.
For his part, Commissioner Chow was reported in the SFGH-JCC’s February 14, 2012 meeting minutes as having requested that DPH explore not only all “possible options,” but that DPH postpone release of the RFP to move dialysis services to LHH until Director of Public Health Garcia reported back to the SFGH JCC regarding this issue.
For her part, Director of Public Health Garcia is not mentioned in public records as having presented a report-back to the Health Commission regarding all options considered before release of the RFP, including an option to move the Renal Center to Building 5. There’s no public records, apparently, that Garcia ever “reported back” before the RFP was issued.
As if the Health Commission didn’t observe that Garcia had gone missing in action, or AWOL, providing the requested report-back.
Perhaps Garcia presented a report-back in a closed-door session of the Health Commission, or by e-mail to Health Commissioners. But dialysis patients, patient advocates and caregivers, and members of the public never heard in public meetings, any or all options the Health Commission requested be explored, or that Garcia may, or may not, have presented.
All
along, the Health Commission, DPH, SFGH, and LHH have played a
really bad circle game, delaying for long over a decade, decisions
on how to provide life-saving dialysis services to San Francisco’s
most vulnerable patients.
The “Life Safety” Canard
Over a decade ago, then Dr. Talmadge King, who oversaw medical services at SFGH, was quoted in the San Francisco Bay Guardian (“Kidney punch,” October 6, 2002) that “There aren’t enough dialysis spots in San Francisco, and we’re very worried about that.”
Considering the glacial speed of rebuilding the Bay Bridge following the Loma Prieta earthquake, and the endless delay of building a safety barrier on Golden Gate Bridge, the decade-long delay in planning for caring for increasing numbers of MediCal-reliant dialysis patients in San Francisco is not too surprising, and was almost predictable.
The
claim is that SFGH’s Building 100 is not life-safety compliant
due to lack of sprinklers, fire alarm speakers, and smoke alarms,
and may have an open stairwell in the building that doesn’t
have a fire-wall door. Ms. Currin’s April 2012 PowerPoint
presentation to the Health Commission noted getting the fire safety
deficiencies, sprinklers, and alarms up to Life Safety code would
cost a mere $636,000, and other improvements another $331,000,
for a total of less than one million dollars. Add to that another
$5.5 million to correct the elevator’s ADA access deficiencies
— which SFGH has long delayed bringing into ADA compliance
and should have been upgraded by now, and which expense it will
eventually have to bend over and cough up — for a total of
just $6.5 million. This is chump change, which DPH surely has.
SFGH’s Renal Center could stay right where it is, and prevent
the fragmentation of dialysis patient’s care. It is thought
that the increased costs of transportation could have easily funded
the first million to correct Life Safety code deficiencies in
Building 100.
But the area proposed for dialysis at LHH also reportedly has an open stairwell — admittedly at the opposite end of the third floor hallway — that also does not have a fire-wall door. And a former staircase immediately adjacent on the right to the entrance area where the LHH dialysis center will be housed, has been removed during reconstruction, limiting egress from the building to a central staircase a good 100 to 200 feet away, at minimum, from the proposed dialysis space, and the open stairwell further down the hallway.
As with the debate of getting CPMC patients out of a third-floor location, getting dialysis patients in wheelchairs, on gurneys, and using other assistive devices down two flights of stairs at LHH during an emergency hasn’t been discussed openly, least of all by the Health Commission. The best life-safety location appears to be in Building 5 — SFGH’s current main hospital — that the Health Commission seems to have forgotten even exists as the best, obvious option, since it is far more seismically safe than either SFGH’s Building 100 or in LHH’s old buildings.
The Other Candards Circle
In addition to patient advocacy concerns about the wisdom of increasing transportation burdens on vulnerable dialysis patients by shunting them to LHH, there are other canards involved.
First, DPH claims insufficient space at SFGH to meet the growing demand of Safety Net patients. DPH ignores the 140,000 square feet of space that will become available in Building 5 in which to “grow” Renal Center space in a centralized care location on the same campus where it has operated for 46 years.
Second, although DPH claims the Renal Center will grow from 13 to 30 chairs by moving it to LHH, dialysis staff have questioned this assumption, since in order to be profitable, the contractor awarded the RFP to operate at LHH will more than likely limit the number of chairs it will contract to DPH to probably 15 chairs, reserving the rest for privately-insured patients in order to develop a payer mix to meet revenue projections and remain profitable. It’s unlikely the 13 current “chairs” will grow by much if the vendor chosen restricts the number of chairs contracted for DPH clients to 15.
Given current trends, the dialysis patient population is expected to grow significantly, and San Francisco will need more and more dialysis chairs to serve MediCal patients, not less.
Third, DPH’s April 10 PowerPoint presentation to the Health Commission indicated that the “current plan is to issue [an] RFP for either a private or non-profit provider.” Health Commissioners Chow and Sanchez stated several times they expected a contract would go to a non-profit provider. Elsewhere, patient advocates were assured the RFP was being developed to award the contract to a non-profit provider, but that restriction wasn’t in the RFP eventually issued. According to a DPH contracting officer on September 25, the only three companies to submit a letter of intent by the August 26 deadline making them eligible to bid on the RFP were from Dialysis Clinic Incorporated (DCI); Satellite Healthcare, Inc.; and DaVita HealthCare Partners, Inc. Only the first two are non-profits; DaVita is a for-profit company. In 2012, there were reports that two for-profit dialysis chains in San Francisco have pending legal actions against them for submitting false billing claims, over-using anemia drugs, and for using dialysis machines associated with infection and death.
CPMC’s
Dialysis Center is now outsourced to Da Vita, which by report
has denied patients oxygen, substituting re-circulated air because
it’s free.
Fourth, of great concern, the RFP restricts the hours of operation for dialysis at LHH to Monday through Friday from 6:00 a.m. to 6:00 p.m., and will exclude holidays “generally recognized by the City.” But SFGH’s Renal Center currently operates from 5:30 a.m. to 8:00 p.m. Monday’s, Wednesday’s, and Fridays, and is open from 5:00 a.m. to 6:00 p.m. on Tuesday’s, Thursday’s and Saturday’s. In effect, the RFP’s restrictions will eliminate at least 26.5 hours of dialysis treatments weekly by curtailing the hours of operation.
Another potential problem may involve water. Hemodialysis requires a lot of water, and water treatment. There are unavoidable leakages, with water flowing down hill into areas below any dialysis unit not located on a ground floor. This may be a problem at LHH, if there is water leakage from a third floor dialysis unit down to Moran Hall on the second floor, or Gerald Simon Auditorium and the Chapel on the first floor. After the $600,000 mold problem that resulted from water leakage in LHH’s new Pavilion Building that the Observer reported in our July issue (“Of Mold and Men”), you’d think LHH would be more cautious about projects with potential water leaks.
Some observers note that violence in dialysis centers is on the rise, and are worried that the RFP says the City will provide building security only at levels currently provided. Other concerns are whether the vendor awarded the contract will have to pay additional rental under the lease if they decide Saturday hours will be needed to meet increases in demand for dialysis services. The RFP also stipulates that electrical usage in excess of the operating hours will also have to be reimbursed by the tenant for any electrical consumption overage.
DPH
claims that operating the Renal Center at SFGH results in a mere
$9,063 annual revenue loss, mostly from the $20,000 monthly it
spends on out-of-network costs for SF Health Plan patients unable
to be accommodated in its current location who are referred to
external providers. DPH also claims revenue to the vendor awarded
the contract to outsource dialysis may potentially earn $1.25
million annually operating a 30-chair dialysis unit at LHH. SFGH
Renal Center staff who have testified before the Health Commission
have noted that outpatient dialysis is a revenue generator for
SFGH, and outsourcing it will result in the loss of millions of
dollars in revenue for SFGH and DPH.
Some observers believe UCSF and SFGH and DPH are simply fudging their facts.
As with the dumping-of-the-elderly problems reported in “Who’s Dumping Grandma?” in the Observer’s June issue, and the dumping-of-mental-health-patients problems reported in “Squished Together: Misery Visits Company” in the Observer’s September issue, it now appears that DPH is dumping dialysis patients over to LHH principally to increase DPH’s revenue under implementation of Obamacare, by swapping out dialysis revenue for the much more stable revenue it will generate by renting out floor space at LHH to an outsourced vendor, dialysis patient’s outcomes be damned.
Welcome to the circle game, which may be a close second-cousin-twice-removed relative of the circle jerk phenomena at the 2012 Democratic National Convention in Charlotte, North Carolina described by the New York Times Magazine’s chief national correspondent, Mark Leibovich, in his new book “This Town” on the New York Times’ current best-seller list.
The Lack of Public Hearings Circle
One remaining question is whether Supervisors David Campos and John Avalos will step up to the plate to have the RFP cancelled, reconsidered, and potentially put out for re-bid, if space cannot be located in Building 5 at SFGH. After all, that vacated space will open up just about the same time that a dialysis center at LHH would open up. The two Supervisors should schedule a hearing to discuss the pros and cons of moving dialysis services to LHH, adversely affecting health outcomes for their constituents.
The
two members of the Board of Supervisors successfully forced Mayor
Ed Lee into re-negotiating with CPMC to build its Cathedral Hill
Hospital on Van Ness Avenue by forcing CPMC to also rebuild St.
Luke’s Hospital in the Mission to prevent the loss of vital,
accessible healthcare services to particularly vulnerable East
Side residents.
The question now is whether Avalos and Campos might step in to prevent the loss of services to patients in the Mission, Bernal Heights, Excelsior, and the Bay View Hunters Point neighborhoods, among others, who would face having their dialysis care outsourced and fragmented to LHH, where the circle-game may come full circle.
After all, if the Health Commission’s Executive Secretary Mark Morewitz is correct — which he is probably not — that the SFGH Renal Center has been “outsourced” to UCSF, a private hospital, despite SFGH actually holding the license for operating it using UCSF staff under is ’affiliation agreement,’ then the Health Commission should have already conducted what is known as a “Prop. Q” hearing to determine whether a private-sector hospital’s abandonment of services will have an adverse, negative effect on the health of San Franciscans. Such a hearing requires a vote by the full Health Commission for private hospitals.
Alternatively, if SFGH decides to reduce the availability of on-site outpatient dialysis services, the County Board of Supervisors are required to hold what is known as a “Bielenson hearing,” which State law requires whenever healthcare services will be reduced at a given County location, or when the transfer of management of a County-operated healthcare facility is being considered, notice must be posted on the entrance doors of the affected facilities, and County supervisors are required to hold a public hearing.
 Neither
a Prop. Q hearing, nor a Bielenson hearing, have been held to
date. One or the other — or both — must apply.
Neither
a Prop. Q hearing, nor a Bielenson hearing, have been held to
date. One or the other — or both — must apply.
It’s time for Supervisors Avalos and Campos, and other Supervisors, including District 7 Supervisor Norman Yee, to interrupt this circle game.
Monette-Shaw is an open-government accountability
advocate, a patient advocate, and a member of California’s
First Amendment Coalition. Feedback: monette-shaw@westsideobserver.com.
The print edition of this Westside Observer article was a condensed
version; this is the expanded version.
Postscript 1: Supervisor David Campos Schedules a Heaing for Thursday, October 17
st as this article was about to
be posted on the Internet, news surfaced that Supervisor David
Campos has scheduled a Neighborhood Services and Safety Sub-Committee
hearing on the outsourcing of SFGH's Renal
Center for Thursday,
October 17 at 10:00 a.m. in Board Chambers, Room 250 at City Hall.
Please plan to attend this hearing to help keep this life-saving
service right where it belongs — at SFGH!
Postscript 2: Upcoming Hearing Notice on Re-Use of Old Laguna Honda Hospital
Readers may want to consider attending on Tuesday, October 15, 2013 at 4:00 p.m., an annual meeting of the Public Health Commission traditionally held at Laguna Honda Hospital in the John Kanaley Community Center meeting room in LHH’s new main entrance called the Pavilion building. The meeting agenda lists presentation of LHH’s annual report, and an update on construction of LHH’s Replacement Project. Health Commissioner Judith Karshmer requested on May 28, 2013 that the full Health Commission receive a presentation to review the planned use for all of the remaining old buildings at LHH initially slated for demolition. There may be a discussion of re-use of the old “finger wings” of the old main hospital for other uses, rather than demolition, but it is not listed as a separate item on the agenda.